- Wellington’s Malaghan Institute is expanding its Car-T cell therapy trial for cancer.
- Over 60 patients will receive the treatment in the trial’s second phase over two years.
- The therapy is a potential game-changer for certain cancers.
A ground-breaking clinical trial that’s made a life-saving difference for Kiwi cancer sufferers is being widened to treat more patients – with growing hopes of the therapy becoming a standard care here.
The Enable trial, run by Wellington’s Malaghan Institute of Medical Research, represents first-of-its-kind technology for New Zealand and a potential game-changer for certain cancers.
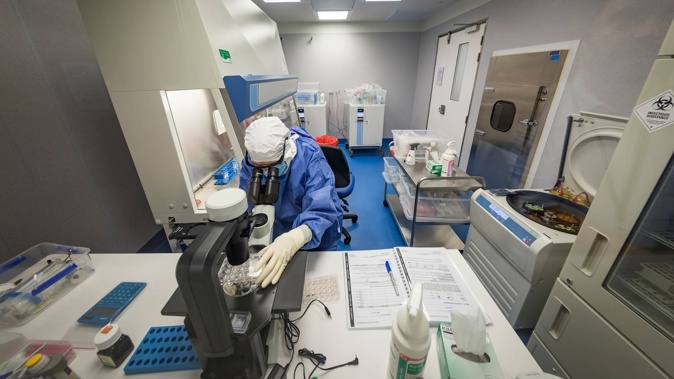
It involves Car-T cell therapy, in which a patient’s immune cells are collected, genetically modified to recognise and kill their cancer, then given back to them as treatment.
Used overseas for types of blood cancers including relapsed lymphoma, leukaemia and myeloma, Car-T therapy isn’t yet available as a funded treatment here.
The researchers behind the trial hope to see that change.
Their locally developed therapy has been found highly effective against its target cancers – B-cell non-Hodgkin lymphomas – while also safer than leading international therapies.
Of 30 patients who took part in the trial’s first phase, after exhausting all other treatment options, more than half were shown to be cleared of cancer just three months later.
Now, the trial is moving ahead to phase 2 and seeking more patients.
“We have final regulatory and ethical approvals, our first site is ready to go, and clinicians around New Zealand have been advised of the criteria and how to refer patients,” Malaghan Institute clinical director Dr Robert Weinkove said.
This time, 60 patients with certain types of relapsed or refractory large B-cell non-Hodgkin lymphoma will be treated over two years, but more quickly than in the trial’s first phase.
“We are hopeful that treating patients earlier – as a second- or third-line therapy – will result in even better Car T-cell outcomes as their immune system function may have been less damaged by their prior cancer treatments,” Weinkove said.
“The safety profile of our new Car T-cell therapy also means we can deliver it as an outpatient treatment, lowering the burden on patients and their whānau, and reducing costs to the health system.”
Leukaemia and Blood Cancer New Zealand chief executive Tim Edmonds told the Herald it was “exciting” to have the trial delivered in Aotearoa.
“For the 60 patients that will be involved, it offers a one-time, potentially curative treatment when they would otherwise require ongoing therapy with the associated risk of relapse and diminishing treatment options,” he said.
“The trial is also an excellent opportunity for our health system to develop the essential capabilities and processes needed to make Car T-cell therapy a standard treatment for all eligible patients in the future.”
For Auckland woman Michele Leggott – today cancer-free some 20 months after receiving the therapy in the trial – news of the second phase was “wonderful”.
“I can say that I’m well and in remission, which is fantastic.”
Collectively, the type of cancers targeted by the new therapy accounted for about 1600 diagnoses here each year, and it was estimated around 200 of those might benefit from the therapy.
While there was potential to push its reach to other subtypes of lymphoma and myeloma, its prospects for treating “solid” cancers – like lung, breast and prostate – weren’t yet as promising.
Malaghan and its start-up company BioOra were meanwhile in talks with the Government and health sector about the therapy’s next steps – while putting in place local manufacturing and delivery measures that could establish it as a standard of care.
Jamie Morton is a specialist in science and environmental reporting. He joined the Herald in 2011 and writes about everything from conservation and climate change to natural hazards and new technology.
Take your Radio, Podcasts and Music with you









