
Breast cancer is the most common form of cancer to affect Kiwi women. For women with the BRCA1 gene mutation, the risk of getting breast cancer rises to 57 per cent. Forty per cent of them develop ovarian cancer by the age of 70.
The statistics are frightening. But they became all too real for one young Kiwi mum who tested positive for the BRCA1 mutation and suddenly faced the possibility that she might not get to see her daughter grow up.
Rather than live each day under threat of a devastating diagnosis, she made the brave decision to have her breasts removed.
She chats to Bethany Reitsma about the factors that went into that tough decision, and why it's important New Zealand women get tested for BRCA1 and know what their options are.
Ten weeks after surgery, Jade Vercoe has just started going to her beloved F45 classes again - but she's avoiding chest workouts.
The mum of one has had both her breasts removed in a prophylactic, or preventative, double mastectomy.
"I'm feeling really good. The first six to eight weeks were difficult, I couldn't pick up my daughter and hold her. I'm still a bit sore and tender but I can't complain," she tells the Herald.
Vercoe tested positive for the BRCA1 (breast cancer 1) gene mutation in 2018 along with several other members of her family, including one aunt who had already had breast cancer twice.
All women carry the BRCA1 and BRCA2 genes, but they can mutate and increase the risk of developing breast and ovarian cancer. Many women who test positive for the gene opt to remove their breasts, which reduces the risk of developing cancer by 95 per cent.
"My sister and I both tested positive for the gene mutation," Vercoe shares.
"I initially had a bit of a cry. My family were pretty upset when I found out I had the gene. It affected my dad a lot because the gene mutation was passed down through him.
"But you realise that it is what it is and you're better off knowing it now. I had a chat with my partner Craig and made the decision to remove my breasts."
So what led the 32-year-old to that decision? For Vercoe, it all came down to being in control of her own life.
"We made the decision early on," she confides. "It's such a high risk of getting breast cancer if you have the gene and I wanted to be in the driver's seat. I didn't want to just wait and see what happens. Now I'm not going to die, I'm not going to get breast cancer, and I got new boobs!" she jokes.
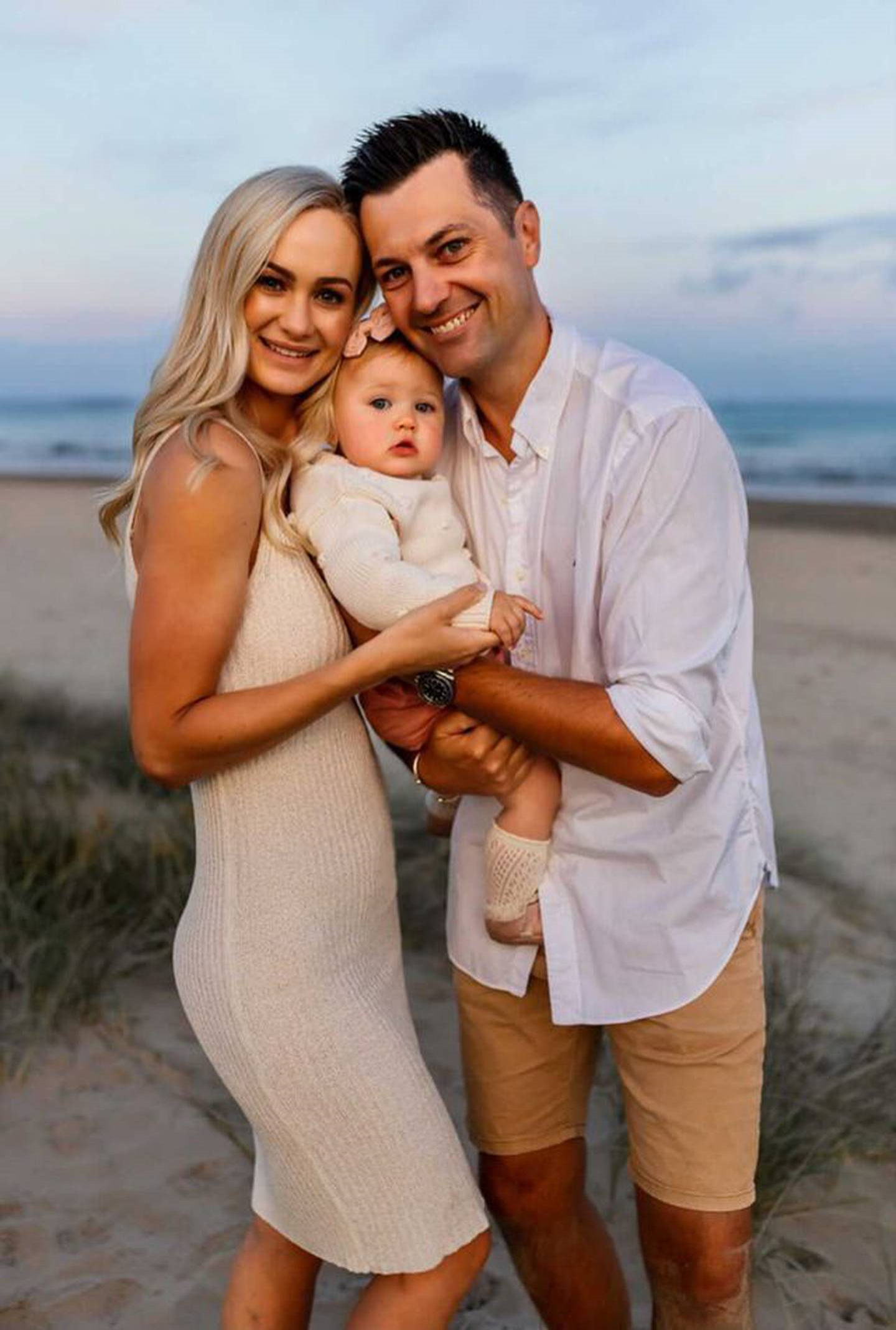
Jade and partner Craig decided to postpone the surgery until they'd had their baby daughter Maddison. (Photo / @jade.vercoe)
And she shares that her family were all "super supportive" of the decision - "we were all very much on the same page".
At the time of her test, she and her partner Craig were thinking about having a baby, so they decided to postpone her surgery until after that. She fell pregnant with baby Maddison in March 2019 and went for six-monthly tests, ultrasounds and mammograms throughout the pregnancy and after her daughter was born.
Although the elective surgery is available through the public hospital system, it comes at a cost in other ways.
"It's a big financial commitment, it's a lot of time off work and hospital visits, we had to put Maddison into full-time daycare," she shares.
Because of her family history with cancer, it was easy for Vercoe to get a referral for surgery - but it's not easy for everyone to get the initial gene testing, she reveals. She'd never even heard of BRCA1 until a few years ago, and she recalls a girl at her F45 gym who just got a referral for testing after waiting for months.
"There's just not enough information or knowledge about it. GPs don't have those conversations with you," she says.

Vercoe says not enough Kiwi women are aware that BRCA1 even exists, let alone that there are surgery options available to them. (Photo / @jade.vercoe)
But when she decided to document her journey on Instagram, going public with the diagnosis, she suddenly had hundreds of women messaging her from around New Zealand and the world about their experiences with BRCA1 and realised she wasn't alone.
Vercoe has had breast implants before, so the procedure wasn't entirely foreign - but it took months to recover.
"I felt really out of it. My chest felt super tight, like there was a truck sitting on it. It's a bit restrictive on your breathing as well - but waking up was this sigh of relief. I'd been counting down the days," she reflects.
The drains in her chest to get rid of excess fluid were the worst part, she says - "they were painful, uncomfy and annoying. The biggest relief was getting them removed.
"And you have to have these tight dressings on called pico dressings. They come with a battery pack that has a pump in it. They vibrate and are also really tight and annoying. Removing these was on day 7 was the best feeling ever."
Four nights in the hospital were followed by physical therapy, starting with simple exercises like shrugging and deep breathing.

Four nights in hospital were followed by a long recovery process and lots of physical therapy. (Photo / @jade.vercoe)
"At first you can't drive, you can't carry items heavier than a full mug. I'm so lucky that Craig works from home because you need that support system around."
But not everyone has the support in place to allow them to have the surgery, as she reveals.
"A single mum got in touch with me, she has BRCA and wanted to have the surgery but she has two kids - financially and physically she couldn't do it, she didn't have that support system.
"It's the little things like, why do we have to pay so much for damn hospital parking? In an ideal world there would be that support so that people who need this can do it."
But there are some perks, she shares. The Ministry of Health provides mastectomy patients with $1200 worth of free surgical or sports bras.
"I wouldn't say no to getting some nice new bras!" she admits.
"I already had minimal breast tissue so I'm a similar size to what I was. They do feel different, a lot firmer and there's next to no feeling in them. For someone with natural boobs this would be a bit of a shock.
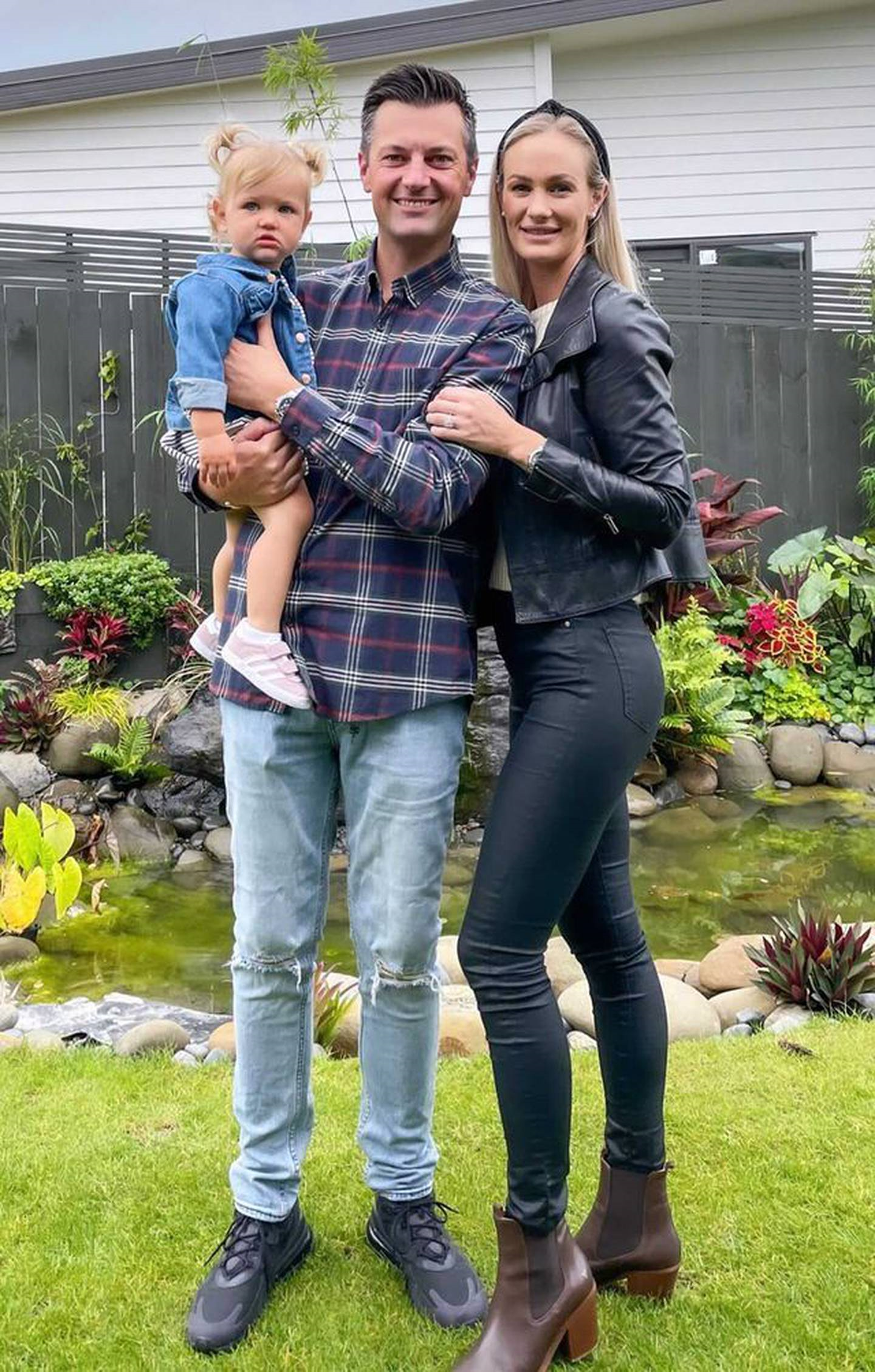
Rather than risk getting cancer, Vercoe chose a future with her partner Craig and one-year-old daughter Maddison. (Photo / @jade.vercoe)
"It takes a bit of getting used to."
Vercoe is still at risk of getting ovarian cancer, but this is harder to pre-empt. She plans to start getting screenings once she turns 40.
"There's no specific testing for ovaries, so you are always living with a ticking time bomb," she says - but while she's living with that time bomb, she still considers herself incredibly lucky.
Reflecting on her journey so far, Vercoe says it's "gut-wrenching" how close she might have come to getting cancer, but she's now focusing on the future.
"It's not just getting your boobs removed, it's a lifetime journey. You have to confront it and then you have to find a way to focus on the positive."
Her decision to have surgery might just have saved her from future heartbreak - and she wants other Kiwi women to know it could save them too.
"I want to make it more of a normal conversation. The important thing is to get awareness out and know that it's okay to talk about it.
"If your family has a history of breast cancer, get on the phone, see your doctor. It could have saved my life. It could save your life."
Take your Radio, Podcasts and Music with you









