
Reports of potentially higher rates of vaccine hesitancy among Māori and Pacific populations have seen the government target Covid-19 vaccine and information campaigns at those communities.
And there are excellent reasons for such a targeted approach, designed and delivered by Māori and Pacific leaders for Māori and Pacific people. More so, given existing inequities within the health-care system that have fostered unequal health outcomes and distrust in health institutions themselves.
But it is also important to confront the inference that Māori and Pacific people are more prone to believe Covid-19 vaccine conspiracy theories, and that this might be the most significant barrier to vaccination uptake.
Using data collected from a diverse sample of New Zealanders, we found no basis for this. When modelling accounts for the key factors we know are associated with vaccine hesitancy, such as education and age, ethnic differences are no longer statistically significant.
That is, differences in vaccine hesitancy rates for Māori and Pacific communities are explained by their younger age structure and lower educational attainment. Indeed, across all communities, these are the main factors associated with vaccine hesitancy.
These findings are, of course, fairly intuitive when we look at the successful leadership from Māori and Pacific communities during the early pandemic response, including initiatives such as a contact tracing card trial and community checkpoints.
The risk of inequitable vaccination rates
The real risk is that the intention to be vaccinated doesn’t translate into actual uptake. Early data on the COVID-19 vaccine rollout suggests fewer Māori and Pacific people are fully immunised.
This matters because these populations have a greater risk of COVID-19 transmission, severe infection, ICU admission or even death.
Despite the Ministry of Health’s phased rollout plan, it seems some populations could be protected sooner than others due to the geographic and other barriers faced by Māori and Pacific people.
This mirrors known trends in health-care access in Aotearoa where services are inequitably distributed. Wealthier, healthier and whiter populations tend to have the best access to facilities and high-quality care.
Time and distance are the real barriers
Our analysis shows that offering vaccination at existing health facilities and pop-up sites would be inequitable. Māori, older people and poorer communities would be disproportionately affected by distance and travel times from where they live.
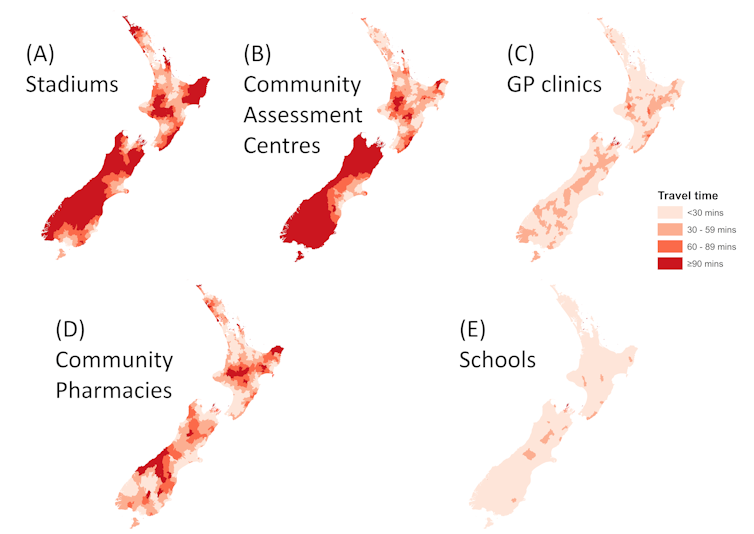 Estimated travel times to five types of potential COVID-19 vaccine delivery site. NZ Medical Journal, Author provided
Estimated travel times to five types of potential COVID-19 vaccine delivery site. NZ Medical Journal, Author provided
Schools and GP clinics are clearly the most easily accessible sites. However, converting schools into vaccination centres might not be feasible. The best option could be combining effective outreach programs with vaccination centres run from GP clinics, Māori providers and Pacific health services.
While some will find ways to overcome access barriers, others won’t have the time, money or resources. These obstacles become mountains if people are already vaccine-hesitant — regardless of ethnicity.
If they postpone or forgo the vaccine altogether it will make existing inequities worse and challenge the overall COVID-19 elimination strategy, especially when borders open and the risk of community transmission increases.
The threat of other infectious diseases
We know many people have deferred routine health care during the pandemic, including childhood immunisation against other infectious diseases. This has happened against a backdrop of already declining immunisation rates among children in general, and among tamariki Māori and Pacific children in particular.
The result has been worsening coverage rates in some regions with persistently low coverage anyway, as people stayed away from primary health-care providers.
Closing the borders and restricting movement to stop COVID-19 transmission also reduced the spread of other infectious diseases. When these controls are lifted the risk of serious childhood disease outbreaks, such as measles and pertussis, will increase.
High childhood vaccination coverage must be prioritised to counter the vulnerability of Māori and Pacific communities to the immediate and long-term burdens of these diseases.
Avoiding a perfect storm
This winter’s influenza immunisation campaign and the MMR (measles, mumps and rubella) catch-up program are particularly focused on young Māori and Pacific adults. The priority is to prevent further devastating outbreaks of measles.
However, the resources currently prioritised for the COVID-19 vaccine campaign inevitably affect other immunisation campaigns.
Communities across Aotearoa may soon face a perfect storm: fewer resources available to address low childhood immunisation rates, delayed influenza protection and MMR catch-ups, and the potential for the inequitable delivery of COVID-19 vaccines.
These factors, combined with increasing freedom of movement, are likely to result in infectious disease spread, particularly in Māori and Pacific communities.
For the health system to be adequately responsive, it should engage Māori and Pacific leadership in the governance, design and delivery of vaccination campaigns. It will require resourcing, monitoring and accountability to build adaptable solutions that ensure community aspirations are met.![]()
Jesse Whitehead, Postdoctoral Researcher, University of Waikato; Kate C. Prickett, Director of the Roy McKenzie Centre for the Study of Families and Children, Te Herenga Waka — Victoria University of Wellington, and Polly Atatoa Carr, Associate Professor, University of Waikato
This article is republished from The Conversation under a Creative Commons license. Read the original article.
![]()
Take your Radio, Podcasts and Music with you









